Introduction
Long-term, low-dose daily antibiotic therapy is the established standard of care for prophylaxis in women with recurrent urinary tract infections (UTIs), as endorsed by national and international guidelines. However, antimicrobial resistance has been directly linked to antibiotic consumption highlighting the need for non-antibiotic alternatives
Aim
The ALTAR trial (alternative to prophylactic antibiotics for the treatment of recurrent urinary tract infections in women compared the efficacy of methenamine hippurate for prevention of recurrent urinary tract infections with the current standard prophylaxis of daily low dose antibiotics.
Patient Profile
- Women aged >18 years with recurrent UTIs, requiring prophylactic treatment.
- Recurrent UTI was defined as at least three episodes of symptomatic UTI in the previous 12 months or at least two episodes in the past six months.
Methods
- Multicentre, open label, randomised, non-inferiority trial.
Study outcomes
- The primary clinical outcome measure was the incidence of symptomatic, antibiotic treated, UTI episodes self-reported by participants over the 12-month treatment period
- Incidence of symptomatic, antibiotic treated UTI in the six months after treatment were secondary outcomes
Results
Primary outcomes
- Incidence of symptomatic, antibiotic treated, UTI episodes self-reported by participants over the 12-month treatment period
- 90 symptomatic, antibiotic treated UTI episodes were reported over 101 person yrs of follow-up in the antibiotic grp
- 141 episodes over 102 person yrs of follow-up in the methenamine Hippurate grp
- The incidence of symptomatic antibiotic-treated urinary tract infections (UTIs) was lower in the methenamine hippurate group (1.38 episodes per person-year) compared to the antibiotic group (0.89 episodes per person-year).
- The upper limit of the 90% confidence interval for the absolute difference (0.49) is below the non-inferiority threshold of one, suggesting that methenamine hippurate can be regarded as non-inferior to antibiotic prophylaxis for the prevention of UTIs.
Figure 1: Incidence of symptomatic antibiotic-treated UTIs
Secondary Outcomes
- In the six-month follow-up period post-treatment, the incidence rate of UTI was lower in the antibiotic prophylaxis group compared to the methenamine hippurate group, with an absolute difference of 0.53 episodes per person year.
- The incidence of microbiologically confirmed UTIs was lower in the antibiotic prophylaxis grp (0.41) than in the methenamine hippurate grp (0.53), with an absolute difference of 0.11.
- Additionally, the rate of microbiologically confirmed UTI episodes was significantly higher in the methenamine hippurate grp (0.86) compared to the antibiotic prophylaxis grp (0.48), resulting in an absolute difference of 0.38.
- A post hoc analysis identified a significantly higher rate in the methenamine hippurate group than in the antibiotic prophylaxis group 14% of 326 samples vs 7% of 323; P=0.0048
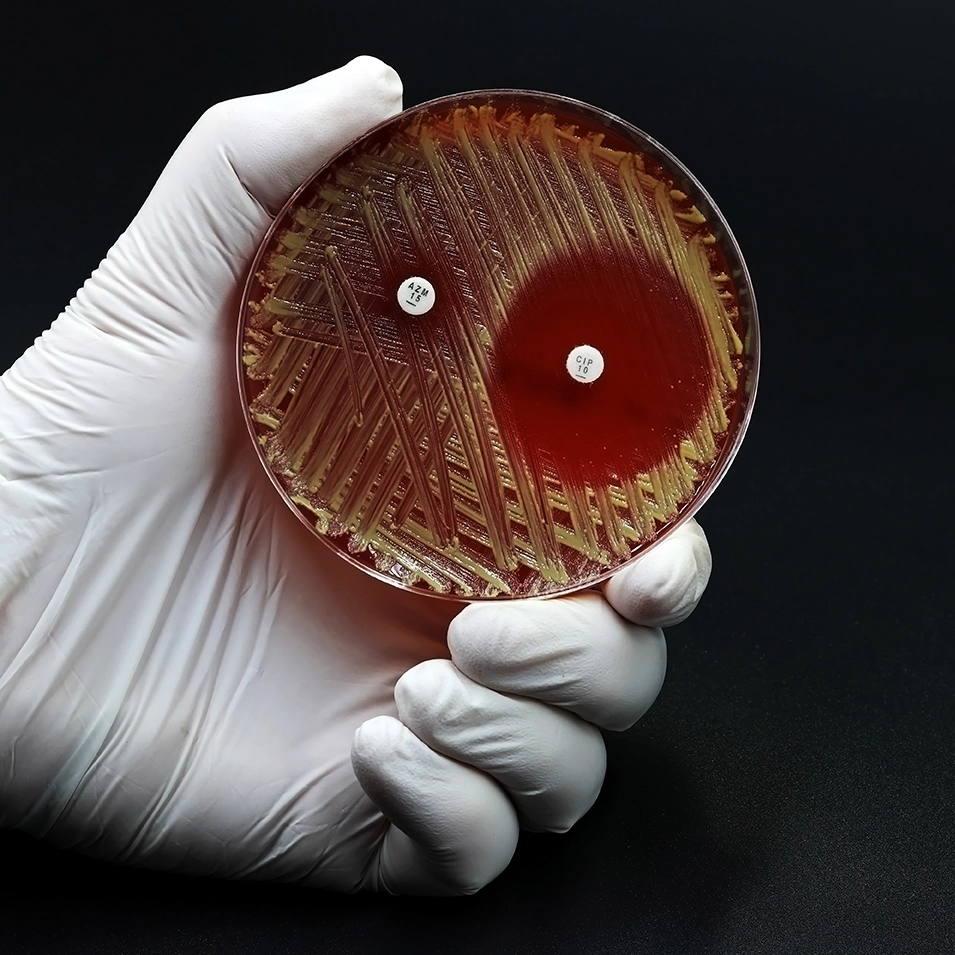
Antimicrobial resistance
- At 6 – 12 month and 18-month follow-up, the antibiotic prophylaxis group exhibited a higher rate of resistance to at least one antibiotic in E. coli from perineal swabs compared to the methenamine hippurate group, while multidrug resistance was more prevalent in the methenamine hippurate group at 18 months.
Figure 2: Proportion of participants with E. coli resistance to at least one antibiotic and multidrug resistance
- Urine cultures results revealed higher rates of resistance to trimethoprim, co-trimoxazole, and cephalosporins in E coli isolated from urine samples from women in the antibiotic arm than in the methenamine hippurate arm.
- Treatment satisfaction was high and comparable between treatment groups, antibiotic prophylaxis group reported higher scores in the convenience domain than the methenamine hippurate group (mean 91.4 v 82.2; t test, P=0.001)
Adverse events
- Rates of adverse events and adverse reactions were low & comparable across treatment groups
- Two serious AEs ie severe abdominal pain and raised alanine transaminase were reported, antibiotic prophylaxis group
- During the 18-month trial, 4 participants on methenamine hippurate required hospitalization for UTIs & 6 reported febrile UTIs with temperatures of 38°C or higher.
Conclusion
The ALTAR trial demonstrated high levels of efficacy of methenamine hippurate in terms of UTI prevention in women with a history of recurrent episodes of urinary tract infections. The elevated antimicrobial resistance rates linked to the antibiotic group, particularly in E. coli, may prompt patients and clinicians to prioritize methenamine hippurate for UTI prevention in women.
Reference
BMJ 2022;376: e068229